
Article reviewed by: Dr. Sturz Ciprian, Dr. Tîlvescu Cătălin and Dr. Alina Vasile
Article updated on: 11-12-2024
Carbon Monoxide Poisoning: Causes, Symptoms and Treatment
- What is carbon monoxide poisoning?
- Causes of carbon monoxide poisoning
- Symptoms of carbon monoxide poisoning
- Risk factors for carbon monoxide poisoning
- Diagnosing carbon monoxide poisoning
- Treatment of carbon monoxide poisoning
- Recovery after carbon monoxide poisoning
- Complications of carbon monoxide poisoning
- Preventive measures for carbon monoxide poisoning
- Myths related to carbon monoxide poisoning
- The difference between CO and CO₂ poisoning
Carbon monoxide, a colorless and odorless gas, is often called the "silent killer" because of the danger it poses without you even realizing it. Exposure to this gas can turn everyday moments, such as using a fireplace or stove, into a serious health risk. Below, you will learn what carbon monoxide poisoning is, where it comes from, and why it is essential to be informed to protect yourself and your loved ones.
What is carbon monoxide poisoning?
Carbon monoxide poisoning is a condition caused by inhaling carbon monoxide (CO), a colorless, odorless, and tasteless gas that results from the incomplete combustion of fuels such as gas, wood, coal, or gasoline. This gas is extremely toxic because it binds to hemoglobin in the blood, reducing the blood's ability to transport oxygen to organs and tissues.
The most common examples of carbon monoxide poisoning include the use of defective or improperly ventilated heating appliances, such as stoves, fireplaces, or boilers; leaving vehicles running in enclosed spaces, such as garages; using portable generators indoors or near windows and doors; grills and camping stoves used in enclosed spaces, such as tents or basements; exposure to smoke from fires, which contains high levels of carbon monoxide; working conditions in industrial facilities, such as factories or mines; chimney blockage by soot or bird nests; and the use of improvised stoves.
Carbon monoxide poisoning can be fatal because the lack of oxygen affects the functioning of vital organs, and in less severe cases, it can leave long-term sequelae, such as memory impairment, concentration difficulties, muscle weakness, persistent neurological and cardiovascular disorders. Carbon monoxide poisoning is the cause of many domestic and industrial accidents, especially during cold months or in emergency situations, such as power outages. Statistics show that annually, thousands of people end up in the hospital or lose their lives due to exposure to this toxic gas. According to data provided by the World Health Organization (WHO) Europe, carbon monoxide proves to be a significant cause of death, with an annual mortality rate of 2.24 per 100,000 inhabitants in Europe. It exceeds HIV/AIDS and skin cancer and approaches the level of deaths caused by alcohol abuse. According to a retrospective study conducted by the National Institute of Public Health (INSP) for the period 2000-2018, deaths caused by carbon monoxide poisoning represent 1.75% of the total autopsies performed and 0.63% of the total violent deaths recorded in Romania.
Carbon monoxide is an extremely dangerous gas, precisely because it is odorless, colorless, and tasteless, making it impossible to detect without special equipment, such as CO detectors. This "silent killer" can invade a space without anyone realizing it, and symptoms often appear too late to prevent serious or fatal effects. The fact that it cannot be perceived with our senses transforms it into an invisible danger, present in homes, vehicles, and industrial spaces, especially in poor ventilation conditions. This invisibility amplifies the risk, especially during sleep, when victims cannot react to early symptoms. Therefore, it is crucial to be aware that carbon monoxide can come from seemingly safe sources, such as improperly used heating appliances, grills, stoves, or generators. The only real protection against this invisible danger is active prevention, including regular maintenance of equipment and the installation of CO detectors, which can save lives through early warning. Ignoring these measures can transform any space into a deadly environment, without any visible sign.
Causes of carbon monoxide poisoning
The most common causes of carbon monoxide poisoning are related to improper or defective use of equipment and devices that involve burning fuels. These include:
- Defective or unventilated heating appliances: Gas stoves, fireplaces, boilers, or heating systems that are not properly maintained or that operate in a space without adequate ventilation.
- Chimney blockage: Bird nests or other obstructions can prevent gas evacuation, causing carbon monoxide to accumulate indoors.
- Portable generators: Using these indoors, such as in homes, garages, or basements, or positioning them too close to open windows and doors.
- Vehicles running in enclosed spaces: Cars left running in garages or other poorly ventilated spaces can quickly release dangerous amounts of CO.
- Grills, camping stoves, or other solid fuel devices: Using these in enclosed spaces, such as tents, basements, or rooms without ventilation, can generate lethal levels of carbon monoxide.
- Fires: Incomplete combustion of materials during a fire produces large amounts of carbon monoxide, which represents a major danger for those exposed.
- Gas leaks: Problems with gas installations, such as cracks in pipes or improperly adjusted burners, can release CO into the air.
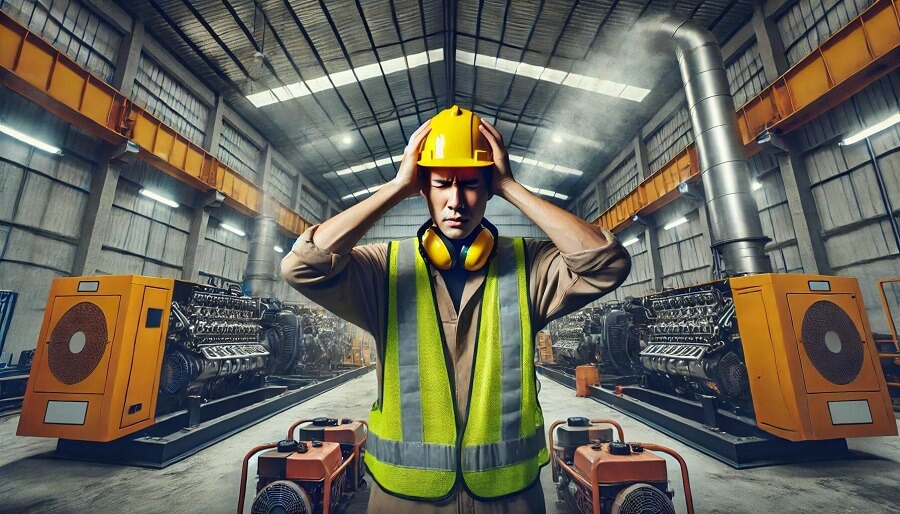
- Industrial equipment: Workers who work in environments with diesel engines, welding equipment, or foundries without adequate ventilation are at increased risk.
- Use of improvised stoves: These are frequently used in emergency periods or poverty and represent a common cause of poisoning.
- Leaks during the use of gas appliances: Ovens or stoves used for heating spaces in unventilated places can produce CO.
Symptoms of carbon monoxide poisoning
Symptoms of carbon monoxide poisoning can vary depending on the level of exposure, the duration of gas inhalation, and the vulnerability of each person. These are often non-specific and can be confused with other conditions, such as the flu or fatigue. People with pre-existing conditions, such as heart disease, lung disease, or anemia, children, the elderly, and pregnant women are more susceptible to the toxic effects of carbon monoxide. The concentration of the gas and the duration of exposure play an essential role in the severity of symptoms, which can evolve from mild manifestations to severe complications if exposure continues.
The first sign of carbon monoxide poisoning is usually a headache. This frequently occurs as an initial symptom and is often described as persistent and moderate-severe, often accompanied by a general state of fatigue.
Mild to moderate symptoms:
- Headaches – frequently the first sign of exposure.
- Dizziness – sensation of imbalance or vertigo.
- Nausea and vomiting – symptoms similar to indigestion.
- Weakness – lack of energy or feeling of extreme fatigue.
- Confusion – difficulties concentrating or unclear thinking.
- Breathing difficulties – feeling of suffocation, especially during exertion.
- Chest pain – often in people with pre-existing heart conditions.
- Tinnitus – noises in the ears.
- Palpitations – accelerated or irregular heart rhythm.
Severe symptoms:
- Loss of consciousness – in severe cases, the person may fall into a coma.
- Seizures – involuntary muscle spasms caused by lack of oxygen in the brain.
- Vision and eye movement impairment – blurred vision or inability to focus.
- Neurological damage – extreme confusion, disorientation, or memory disorders.
- Sudden death – in case of exposure to very high concentrations of CO.
Chronic vs. acute exposure: Exposure to low levels of CO over the long term can cause symptoms such as fatigue, headaches, or irritability, which are harder to identify and diagnose than severe acute poisonings.
If you have any of the symptoms of carbon monoxide poisoning, the first step is to immediately go outside, to a well-ventilated area, to breathe fresh air. If possible, turn off the suspected source of gas, but only if you don't put your safety at risk. It's important to notify other people in the space so that everyone evacuates the affected area. Immediately contact emergency services by calling 112 to receive medical help and report the problem. Do not return to the contaminated space until professionals confirm it is safe. Even if the symptoms seem to improve after you've moved away from the source, consult a doctor, as carbon monoxide poisoning can have serious effects, including complications that are not immediately evident. A prompt reaction can make the difference between a complete recovery and severe health problems.
Delayed symptoms (post-poisoning syndrome):
- Memory problems – short-term memory loss.
- Mood disorders – anxiety, depression, or irritability.
- Motor difficulties – poor coordination or tremors.
- Persistent cognitive impairment – long-term concentration difficulties.
Risk factors for carbon monoxide poisoning
Risk factors for carbon monoxide poisoning include both aspects related to environment and equipment, as well as personal factors that can increase a person's susceptibility to the effects of this toxic gas.
Factors related to environment and equipment:
- Poor ventilation: Enclosed or poorly ventilated spaces increase the risk of carbon monoxide accumulation, especially in the presence of combustion sources.
- Defective heating appliances: Stoves, fireplaces, boilers, or other unmaintained or faulty equipment can emit CO.
- Use of generators and grills indoors: These are common sources of CO in spaces such as basements, garages, or tents.
- Chimney blockage: Obstructions caused by soot, bird nests, or other debris can prevent the evacuation of toxic gases.
- Lack of CO detectors: The absence of these devices increases the risk of unaware exposure.
Personal factors that increase susceptibility:
- Age: Young children and the elderly are more vulnerable due to different metabolism and reduced ability to eliminate CO from the body.
- Pregnancy: Pregnant women are more susceptible, and exposure can seriously affect the fetus, causing hypoxia or other complications.
- Pre-existing medical conditions: People with heart disease, lung disease, or anemia are more sensitive to the effects of carbon monoxide because their ability to transport oxygen is already compromised.
- Occupational exposure: Workers in industrial environments, such as mines, foundries, or factories, are exposed to higher levels of CO, especially if ventilation is inadequate.
- Habits or unforeseen situations: Excessive alcohol consumption or deep sleep in contaminated spaces increase the risk because early symptoms may be ignored or overlooked.
Seasonal conditions:
The risk increases significantly during cold months when the use of heating appliances and improvised stoves is more frequent. This combination of factors can lead to incidents that would be avoided through proper maintenance and increased attention to combustion sources.
Every autumn, after the vineyard harvest, carbon monoxide produced in the fermentation process can accumulate in front of barrels filled with must. This danger is often underestimated, especially in enclosed spaces such as cellars or basements, where fermentation releases gases that can become lethal in a short time. Carbon monoxide, being odorless and colorless, makes these places seem safe, but high concentrations can cause rapid poisoning symptoms, such as dizziness, weakness, or even loss of consciousness. It is essential that people involved in the winemaking process are aware of this risk, properly ventilate the spaces, and limit the time spent in such environments to avoid accidents.
Similar situations are encountered in cellars used for distillation, where incomplete combustion of fuels or accumulation of gases released during the process can significantly increase the risk of carbon monoxide poisoning. Also, smoking chambers represent another dangerous example, especially when stoves or smoke sources are used without adequate ventilation.
Increased risk for young children
Young children are particularly vulnerable to carbon monoxide poisoning due to their rapid metabolism, which leads to greater absorption of the gas, and reduced ability to eliminate toxins. Their symptoms can be more severe and appear more quickly, highlighting the importance of protection and preventive measures, especially in poorly ventilated spaces.
Diagnosing carbon monoxide poisoning

Early diagnosis of carbon monoxide poisoning is crucial, as delayed treatment can lead to severe complications, including permanent injury or death. People suspected of CO poisoning should immediately receive oxygen therapy and be closely monitored. Diagnosing carbon monoxide poisoning is done through a combination of clinical evaluation and laboratory tests, as follows:
- Patient history and symptoms: The doctor analyzes the patient's history, including exposure to potential sources of carbon monoxide, such as defective heating appliances, generators, or fires. Common symptoms, such as headaches, dizziness, nausea, weakness, or loss of consciousness, are a first indication.
- Physical examination: Clinical signs, such as confusion, cherry-red skin (rarely present and only in severe cases), or breathing difficulties, may suggest poisoning.
- Measuring the level of carboxyhemoglobin (COHb) in the blood: This is the standard confirmation test. An arterial or venous blood sample is collected, and a high level of COHb indicates the presence of carbon monoxide. In healthy people, normal COHb levels are below 2%, and in smokers, they can be up to 10%. Any value above these limits indicates exposure to CO.
- Pulse oximetry with CO specificity: Some modern pulse oximetry devices can directly measure the level of carboxyhemoglobin, providing a rapid detection method without requiring blood collection.
- Arterial blood gas analysis: This test evaluates blood oxygen, carbon dioxide, and pH levels, indicating tissue hypoxia caused by poisoning.
- Monitoring other parameters: In severe cases, doctors may evaluate cardiac and neurological functions, as CO poisoning can affect the heart and brain.
- Medical imaging (in severe cases): In cases of severe poisoning, investigations such as brain MRI can identify neurological lesions or cerebral edema caused by hypoxia.
Standard oxygenation tests, such as those done with a pulse oximeter (a device that measures blood oxygen through a sensor attached to the finger), can give misleading results in the case of carbon monoxide poisoning. The pulse oximeter shows how "full" the hemoglobin in the blood is, but it cannot differentiate between oxygen bound to hemoglobin (which is beneficial) and carbon monoxide bound to hemoglobin (which is toxic).
Carbon monoxide has an extremely strong "adherence" to hemoglobin, about 240 times greater than oxygen. Once it enters the body, CO rapidly binds to hemoglobin, leaving less room for oxygen. The problem is that the pulse oximeter "sees" carboxyhemoglobin (hemoglobin bound to carbon monoxide) almost the same as oxyhemoglobin (hemoglobin bound to oxygen). So, although the patient may suffer from a severe lack of oxygen in tissues, the device may indicate a normal oxygen level, which can mislead doctors or rescuers. In other words, the pulse oximeter does not "understand" that hemoglobin is blocked by carbon monoxide and cannot transport oxygen where needed. Therefore, a patient poisoned with CO may have apparently normal readings, although the brain, heart, and other organs are deprived of oxygen.
To correctly verify the situation, special tests are needed, such as a blood analysis that directly measures how much carbon monoxide is bound to hemoglobin (carboxyhemoglobin). These tests show exactly how severe the poisoning is and help choose the appropriate treatment. Therefore, it is essential that doctors do not rely solely on the pulse oximeter when suspecting carbon monoxide poisoning.
Treatment of carbon monoxide poisoning

Hyperbaric oxygen therapy (HBOT) is an advanced and extremely effective method for treating moderate and severe cases of carbon monoxide poisoning, being considered a standard of treatment in such situations. This involves placing the patient in a pressurized chamber, where they breathe pure oxygen (100%) at a pressure of 2-3 absolute atmospheres, accelerating the elimination of carbon monoxide from the blood. Hyperbaric oxygen therapy reduces the half-life of carboxyhemoglobin from 4-6 hours (in normal air) to only 20-30 minutes and delivers oxygen directly to tissues through blood plasma, which ensures adequate oxygenation even when hemoglobin is blocked by carbon monoxide. At the same time, the therapy reduces inflammation, minimizes oxidative stress, prevents neurological and cardiovascular lesions, and helps restore microcirculation, protecting the vital functions of the body.
How HBOT works in cases of carbon monoxide poisoning
- Rapid elimination of CO from blood: Carbon monoxide binds to hemoglobin to form carboxyhemoglobin (COHb), blocking oxygen transport to tissues. Hyperbaric therapy increases the partial pressure of oxygen in the blood.
- Increased tissue oxygenation: HBOT not only eliminates CO but also delivers oxygen directly to affected tissues. During therapy, oxygen is dissolved in plasma in a sufficient quantity to support cell functioning even in the complete absence of oxygen bound to hemoglobin.
- Reduction of oxidative stress and inflammation: Prolonged exposure to CO can lead to oxidative stress and inflammation in tissues, especially in the brain and heart. Hyperbaric oxygen helps reduce these effects, protecting cellular structures.
Numerous scientific studies, such as "Hyperbaric Oxygen Therapy for Acute Carbon Monoxide Poisoning", conducted by Weaver and collaborators and published in The New England Journal of Medicine in 2002, have evaluated the effectiveness of hyperbaric oxygen therapy in treating carbon monoxide poisoning. The results of this study showed that patients treated with HBOT had a significantly lower incidence of cognitive sequelae compared to those who received oxygen administered at normal atmospheric pressure, thus highlighting the benefits of hyperbaric therapy in reducing long-term neurological risks.
Regarding carbon monoxide poisoning and the use of hyperbaric oxygen therapy (HBOT), there are several essential aspects to consider:
- Time is essential: The effectiveness of HBOT decreases with the passage of time from exposure to carbon monoxide. Treatment must be started as quickly as possible to prevent irreversible lesions, especially at the cerebral level.
- HBOT vs. standard oxygen therapy: Although 100% oxygen administered through a mask is effective in mild and moderate cases, HBOT is necessary to accelerate the process of eliminating CO in severe cases or when there are signs of systemic involvement.
- Indication for HBOT: It is used especially in severe cases, such as those with high levels of carboxyhemoglobin (>25% or >15% in pregnant women), loss of consciousness, neurological symptoms (confusion, seizures), or cardiovascular impairment (arrhythmias, chest pain).
- Benefit in preventing brain injury: HBOT reduces the risk of long-term neurological impairment, such as memory loss or post-poisoning syndrome, caused by severe hypoxia and oxidative stress induced by carbon monoxide.
- Protection of the heart and brain: Carbon monoxide strongly affects oxygen-dependent organs. HBOT provides additional oxygen directly to tissues through blood plasma, protecting the heart and brain from ischemic injury.
- Number of sessions required: Usually, a single session may be sufficient for moderate cases. However, severe cases or those with persistent symptoms may require 2-3 sessions to ensure complete elimination of CO and restoration of tissue oxygenation.
- Utility in pregnant women: The fetus is particularly vulnerable to carbon monoxide because fetal hemoglobin has a higher affinity for CO than adult hemoglobin. HBOT protects both mother and fetus, reducing the risks of fetal hypoxia.
- Effectiveness in prolonged poisonings: In the case of prolonged exposure to carbon monoxide, HBOT not only eliminates the gas from the blood but helps repair tissues affected by hypoxia, reducing inflammation and oxidative stress.
- Post-HBOT monitoring: Even after treatment, patients should be monitored for delayed symptoms, such as memory or cognitive disorders, as the effects of carbon monoxide can appear a few hours or even days later.
Before starting hyperbaric therapy, it is important to know the differences between medical hyperbaric chambers (HBOT) and those for cosmetic use (mHBOT). HBOT chambers are certified for medical use, use pure oxygen at pressures of up to 3 ATA, and are operated in authorized clinics, under the supervision of qualified personnel. These treat serious conditions, such as carbon monoxide poisoning, with clinically proven effectiveness. mHBOT chambers, used in salons or spas, operate at lower pressures, without medical supervision, and are not suitable for complex treatments. Choosing medical chambers is essential for safety and effective results.

An example of professionalism and quality in the field of hyperbaric therapy is Hyperbarium Clinic in Oradea, one of the most advanced and modern hyperbaric medicine centers in Romania. With an area of over 3,000 square meters, the clinic offers state-of-the-art treatment conditions in a modern and well-equipped space. The clinic's staff is trained and certified according to European standards, thus ensuring the safety and efficiency of treatments. The medical team is coordinated by Dr. Ciprian Sturz, medical director and surgeon with specializations in general surgery, visceral and emergency surgery, having extensive experience in hyperbaric medicine. The clinic provides the latest technologies and a friendly environment for patients, being a reference point in the field. For more information about hyperbaric therapy and its benefits, we invite you to consult the complete guide or to schedule a consultation.
Other treatments used in severe cases of carbon monoxide poisoning include controlled hyperventilation therapy, which accelerates the elimination of gas from the body through intensive mechanical ventilation, hemoperfusion therapy, which filters the blood to remove toxins, and blood transfusion, rarely used but effective, replacing affected hemoglobin with healthy blood capable of transporting oxygen.
Recovery after carbon monoxide poisoning
Complete recovery after carbon monoxide poisoning is possible in most cases, but for severe cases, medical support and appropriate rehabilitation are essential to reduce the risk of permanent sequelae. Recovery depends on the severity of the poisoning, the time until treatment initiation, and the complications that arise. Here are the key aspects:
-
Immediate recovery:
- Acute symptoms, such as headaches, dizziness, and nausea, usually disappear within a few hours or days after treatment.
- Oxygen treatment (normobaric or hyperbaric) helps rapidly eliminate carbon monoxide and restore tissue oxygenation.
-
Neurological recovery:
- In severe cases, patients may develop cognitive disorders (memory, attention, concentration) or delayed neurological syndrome, which can appear days or weeks after exposure.
- Recovery may include occupational therapy, neuropsychological rehabilitation, and cognitive exercises.
-
Physical recovery:
- Muscle weakness, tremors, or motor difficulties may require physical therapy to regain strength and coordination.
- Gradual and supervised physical activity is recommended for returning to normal routine.
-
Cardiac recovery:
- If carbon monoxide has affected the heart (e.g., arrhythmias, ischemia), cardiological monitoring and treatments may be necessary.
- Recovery may involve medications or lifestyle changes to protect heart function.
-
Psychological support:
- Depression, anxiety, or emotional disorders are common after severe poisoning. Psychotherapy or counseling helps manage these issues.
-
Long-term recovery:
- For some people, complete recovery may take several months, especially if there are neurological or cardiac complications.
- Regular medical evaluations help monitor progress and adjust treatments.
Complications of carbon monoxide poisoning

Complications of carbon monoxide poisoning are diverse and can affect multiple organs. Careful monitoring and appropriate treatment are essential to reduce the risk of permanent sequelae and ensure complete recovery.
Neurological complications:
- Delayed neurological syndrome (DNS): memory loss, confusion, concentration difficulties, severe cognitive disorders.
- Permanent brain injuries: neuronal death that can lead to motor disorders, tremors, or partial paralysis.
- Speech (aphasia) and coordination disorders.
- Seizures and acute cerebral edema due to prolonged hypoxia.
- Cerebral ischemia with impairment of cognitive functions and sensory perception.
- Vascular dementia or other forms of progressive cognitive deterioration.
Cardiac complications:
- Myocardial ischemia: severe impairment of blood flow to the heart, leading to chest pain or myocardial infarction.
- Cardiac arrhythmias: irregular heartbeats, which can increase the risk of cardiac arrest.
- Cardiomyopathy: deterioration of the heart muscle due to hypoxia.
- Severe hypotension, which can contribute to multi-organ failure.
Respiratory complications:
- Acute respiratory failure: the inability of the lungs to oxygenate blood.
- Alveolar and bronchial impairment, especially in cases associated with smoke inhalation.
- Pulmonary edema: accumulation of fluid in the lungs due to vascular lesions.
Muscular and tissue complications:
- Rhabdomyolysis: destruction of skeletal muscles, which releases myoglobin into the blood and can affect the kidneys.
- Tissue necrosis: death of tissues due to lack of oxygen.
- Impairment of extremities through local ischemia.
Renal complications:
- Acute renal failure secondary to rhabdomyolysis or hypoxic shock.
- Impairment of renal filtration, leading to accumulation of toxins in the body.
Psychological complications:
- Severe depression and long-term anxiety.
- Post-traumatic stress disorder (PTSD), especially in cases where poisoning was traumatic.
- Irritability, personality changes, and loss of interest in daily activities.
Metabolic complications:
- Metabolic acidosis: excessive accumulation of lactic acid due to hypoxia.
- Electrolyte imbalances, especially in cases of renal impairment.
Complications in pregnant women and fetuses:
- Severe fetal hypoxia that can cause miscarriage or intrauterine death.
- Irreversible brain injuries to the fetus.
- Intrauterine growth delays and impairment of neurological development.
Systemic complications:
- Circulatory shock: lack of adequate blood flow to organs, leading to multi-organ failure.
- Impairment of microcirculation, which affects tissue regeneration.
Long-term complications:
- Chronic fatigue and decreased resistance to physical effort.
- Hypersensitivity to extreme temperatures due to impairment of the circulatory system.
- Increased risk of cardiovascular or cerebrovascular diseases.
Prompt treatment with hyperbaric oxygen and careful monitoring after carbon monoxide poisoning can reduce the risk of these complications. Hyperbaric oxygen therapy (HBOT), in particular, offers significant advantages in severe cases, accelerating the elimination of carbon monoxide from blood and reducing the risk of neurological and cardiovascular sequelae. Choosing this therapy, when indicated, can make the difference between complete recovery and long-term complications.
Preventive measures for carbon monoxide poisoning

Detecting carbon monoxide poisoning through symptoms is unreliable, as symptoms such as headaches, dizziness, or nausea are non-specific and can be confused with other conditions. In the absence of a clear signal, prevention becomes essential to avoid dangerous exposure. The most effective method of detection and prevention is the installation of carbon monoxide detectors, which constantly monitor the level of gas and emit an alarm if it becomes dangerous. Also, regular checking of appliances that use fuels, such as stoves or boilers, and maintaining adequate ventilation are key measures to prevent the accumulation of carbon monoxide. In this way, the risk of exposure can be reduced before symptoms appear. Do not leave vehicles running in garages or other poorly ventilated spaces, and must fermentation and food smoking should only be done in well-ventilated areas.
Awareness of the dangers and recognition of poisoning symptoms, along with educating family and colleagues, contribute to reducing risks. Following these measures can protect health and prevent serious incidents. The General Inspectorate for Emergency Situations (IGSU) has developed simple and accessible educational materials for children, which include clear rules about how to recognize a risk situation and how to act. These guides are designed to teach children to:
- Identify carbon monoxide detector alarms.
- Not play with heating appliances or fire sources.
- Inform an adult if they feel unwell or detect unusual odors (even though carbon monoxide is odorless, this habit increases general vigilance).
- Learn visible warning signs, such as yellow flame or excessive smoke from a stove, which may indicate incomplete combustion.
The General Inspectorate for Emergency Situations has developed a national platform dedicated to informing the public about how to behave in case of emergency situations, accessible at https://fiipregatit.ro. In addition to this, IGSU provides a free mobile application, available for download in the App Store and Google Play, offering quick access to information and useful tips for citizens' safety.
Myths related to carbon monoxide poisoning
- Myth 1: Carbon monoxide has an odor, so I can detect it. Carbon monoxide is completely odorless, colorless, and tasteless, making it impossible to detect without a special detector. The idea that you can "feel" the presence of CO is false and dangerous.
- Myth 2: If I don't feel sick immediately, I'm not in danger: Symptoms can appear gradually, and prolonged exposure even at low levels can cause serious problems. The absence of immediate symptoms does not mean there are no risks.
- Myth 3: Only defective appliances produce carbon monoxide: Any appliance that burns fuel (stoves, boilers, fireplaces) can produce carbon monoxide, even if it works correctly, if it is not used in a well-ventilated space.
- Myth 4: Smoke detectors also detect carbon monoxide: Smoke detectors and carbon monoxide detectors are different. A specific detector for CO is necessary to monitor the levels of this gas.
- Myth 5: Opening a window always eliminates the risk. Although ventilation can help, it does not always eliminate the accumulation of CO. The source of emissions must be stopped or repaired to completely eliminate the danger.
- Myth 6: Carbon monoxide poisoning only happens in the cold season. Although risks increase in winter when heating sources are used more frequently, poisonings can also occur in summer, for example, from using grills in enclosed spaces or portable generators.
- Myth 7: Carbon monoxide only affects the lungs: Carbon monoxide affects the entire body, especially the brain and heart, by blocking oxygen transport in the blood.
- Myth 8: Only old houses present risks: Any home, regardless of age, can have problems if appliances that use fuels are not properly maintained or ventilated.
- Myth 9: A low level of carbon monoxide is not dangerous: Exposure to small levels of CO over long periods can cause chronic fatigue, dizziness, and other health problems.
- Myth 10: I don't need a detector if I take care of appliances. Even well-maintained appliances can generate CO, and detectors are the only safe method to prevent accidental poisoning.
The difference between carbon monoxide and carbon dioxide poisoning
Carbon monoxide (CO) poisoning and carbon dioxide (CO₂) poisoning differ significantly, especially regarding detection. Carbon monoxide is extremely dangerous because it is odorless, colorless, and tasteless, making it impossible to detect without a special detector. In contrast, carbon dioxide, although also colorless and odorless, can be perceived at high concentrations through its physical effects, such as accelerated breathing, a feeling of suffocation, or dizziness, caused by the displacement of oxygen from the air. The major difference is that carbon monoxide is an "invisible killer," because people do not have the necessary senses to perceive it, which makes CO detectors absolutely essential.
Conclusion:
Carbon monoxide poisoning is an invisible danger, but completely preventable through simple measures: installing CO detectors, maintaining appliances that use fuels, and awareness of risks. Rapid detection and appropriate treatment can save lives, and education in family and community plays an essential role in preventing accidents. Active prevention is the key to avoiding this "silent killer."




