
Article reviewed by: Dr. Sturz Ciprian, Dr. Tîlvescu Cătălin and Dr. Alina Vasile
Wounds That Do Not Heal - Causes, Symptoms, and Treatment
- What does a wound that does not heal look like?
- Examples of wounds that do not heal:
- Symptoms of wounds that do not heal:
- What are the causes of wounds that do not heal?
- What are the risk factors for wounds that do not heal?
- How are wounds that do not heal diagnosed?
- What are the treatments for wounds that do not heal?
- Complications that may arise from wounds that do not heal
- Prevention methods for wounds that do not heal
Wounds that do not heal represent a major challenge for many people and can signal serious health problems. While most wounds heal naturally within a few weeks, some persist, becoming slow-healing wounds, causing discomfort and increasing the risk of infections or complications. These slow-healing wounds, or in some cases, wounds that do not heal at all, are not just a source of frustration, but they can significantly impact the quality of life. In the following sections, we will explore the various causes of these wounds, how they affect the recovery process, and what treatment options are available to promote healing and prevent long-term complications.
What does a wound that does not heal look like?
A wound that does not heal can have a distinctive appearance, setting it apart from a normal healing wound. Typically, the area around the wound is red and inflamed, with redness potentially intensifying over time. The wound edges may darken, turning purple or blue, indicating poor blood circulation. Instead of closing gradually, you may notice that the size of the wound remains the same or even increases. The surface of the wound may be covered with necrotic tissue, which appears black or brown, and there may be discharge ranging from clear to purulent, often accompanied by an unpleasant odor. In some cases, the wound may bleed slightly when touched, and the pain may be constant or intensified, indicating an infection or ongoing tissue damage.
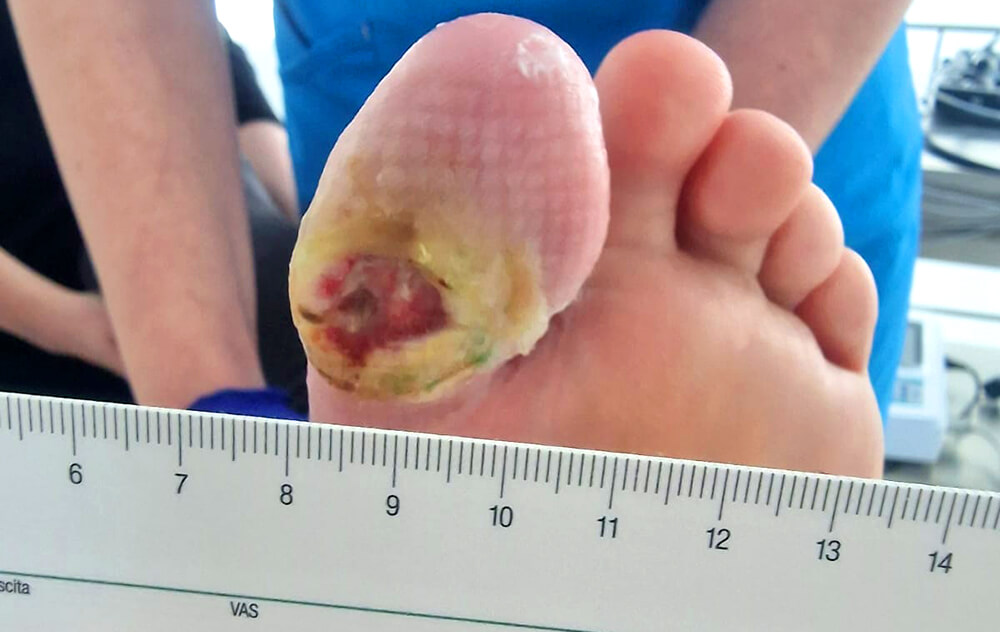
Examples of wounds that do not heal:
Chronic wounds or wounds that do not heal normally are often encountered in various medical conditions. Here are some of the most common types:
-
Diabetic ulcers: These occur in people with diabetes, usually on the feet, and are caused by neuropathy and poor blood circulation.
-
Pressure ulcers (bedsores): These wounds occur in immobile people due to constant pressure on certain areas of the body, such as the hips, back, and heels.

-
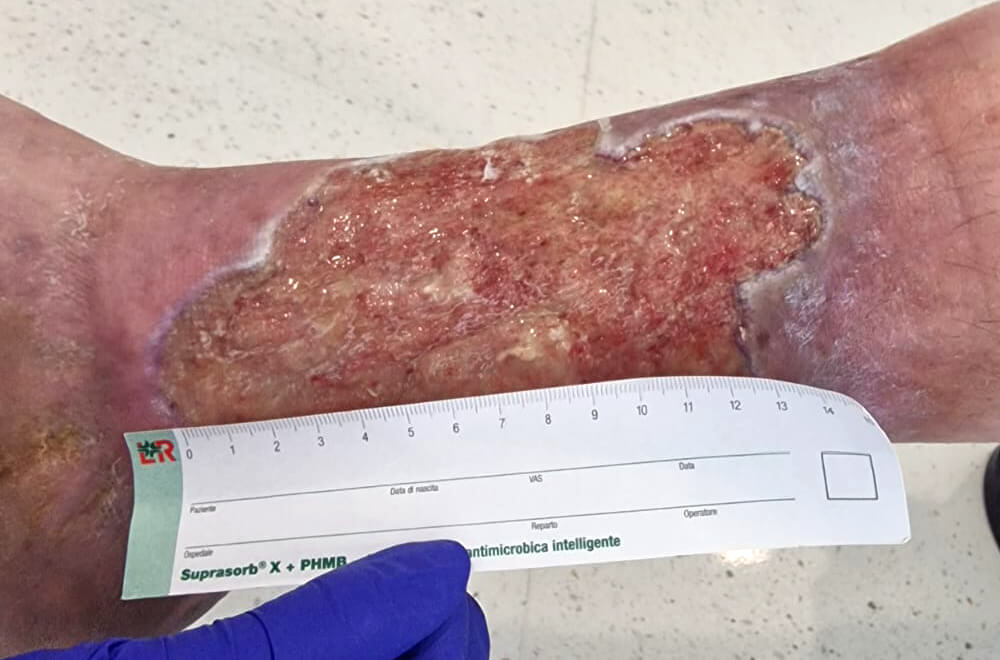
Venous ulcers: These often develop on the legs due to chronic venous insufficiency, which impedes normal blood circulation.
- Radiation therapy wounds: These can occur after radiation treatments due to tissue and blood vessel damage in the irradiated area.
-
Surgical wounds: Some post-operative wounds do not heal properly due to infections or other complications, such as diabetes or malnutrition.

- Traumatic wounds: These include severe injuries such as open fractures and burns, which can become chronic if not treated properly.
- Arterial ulcers: These wounds occur due to extremely poor blood circulation, usually in people with peripheral artery disease, and often develop on the legs.
- Oncological wounds: In cancer patients, some tumors can lead to the development of chronic skin wounds, known as tumor ulcerations, which are difficult to treat.
-
Mixed wounds: Sometimes chronic wounds can have multiple causes, such as a combination of venous insufficiency and artery disease, complicating treatment and healing.

Symptoms of wounds that do not heal:
If you notice any of these symptoms, it is essential to consult a specialist to assess the wound and determine the appropriate treatment. Ignoring these signs can lead to serious complications, such as severe infections or even loss of functionality in the affected area:
- Increased redness or inflammation around the wound;
- Pain that does not improve or continues to worsen;
- Discharge from the wound, which may or may not have an unpleasant odor;
- Dark purple or blue color around the wound edges;
- Persistent swelling in the wound area, which may be a sign of ongoing inflammation or fluid accumulation;
- Constant bleeding or recurrence of bleeding, even with minimal trauma;
- Increasing size of the wound instead of shrinking, which may suggest an infection or further tissue damage;
- Formation of necrotic tissue (dead tissue), appearing as a black or brown area on the wound surface;
- Loss of sensation around the wound, which may indicate nerve damage, commonly seen in people with diabetes;
- Significant slowing of the healing progress after an initial period of improvement, suggesting that the healing process has stalled or regressed.
What are the causes of wounds that do not heal?
Non-healing wounds can have several causes, each contributing to the delayed healing process in different ways:
- Infections can prevent tissue regeneration and worsen the wound, making it take longer to heal.
- Circulation problems, such as those found in people with cardiovascular diseases, reduce blood flow and nutrients to the affected area, slowing the healing process.
- Advanced age can slow the healing rate due to the body's decreased regenerative functions.
- Repeated trauma to a wound can keep it open and irritated, making healing even more difficult.
- A weakened immune system, whether due to illness or other reasons, can reduce the body's ability to fight infections and repair tissues, prolonging healing.
- A history of smoking negatively affects circulation and tissue oxygenation, and certain medications can also disrupt the natural healing process.
- Diabetes affects circulation and immunity, making wounds harder to heal.
- Poor nutrition can slow healing because the body does not receive the necessary nutrients for tissue regeneration.
- Constant pressure on a part of the body can impede blood flow, leading to pressure ulcers, or bedsores, which are difficult to treat.
- Obesity can place additional pressure on certain parts of the body and affect circulation, contributing to delayed healing.
- Anemia can lead to slower healing due to a lack of oxygen in the tissues.
- Dehydration affects the skin's elasticity and regenerative capacity, prolonging the healing process.
- Radiation or chemotherapy can affect the skin and tissues, slowing or preventing wound healing.
These are just some of the possible causes that can make a wound chronic and require additional medical care. These factors can act individually or in combination, making wounds chronic and difficult to treat.
What are the risk factors for wounds that do not heal?
One of the main factors is diabetes, which increases the risk of chronic wounds, especially on the feet. This is due to reduced blood circulation and neuropathy, which can hinder proper healing.
Circulatory problems, such as peripheral artery disease or venous insufficiency, can limit blood flow to the affected area, preventing the delivery of essential oxygen and nutrients for healing. Older people are also more prone to such problems, as the skin becomes thinner and less elastic, and the body's ability to repair damaged tissues decreases with age.
Long-term immobility is another risk factor, especially for the development of bedsores, as constant pressure on certain areas of the body can damage the skin and underlying tissues. Infections are another obstacle to healing, as they can destroy tissues and complicate the natural repair process.
Immune deficiencies, such as HIV/AIDS, compromise the immune system and reduce the body's ability to fight infections and repair tissues. Exposure to radiation, especially in cancer treatments, can damage the skin and blood vessels, affecting healing in the treated area.
Additionally, chronic stress plays a significant role, as it can affect the functioning of the immune system and lead to the production of stress hormones that interfere with cellular regeneration. All these factors, whether acting alone or in combination, can significantly delay the wound healing process.
How are non-healing wounds diagnosed?
For a patient who suspects they have a non-healing wound, there are a few essential things to know. First, it is important not to ignore the problem. A wound that does not heal within a few weeks should be evaluated by a doctor, as it may indicate an underlying health issue, such as diabetes, circulatory problems, or an infection.
The patient should watch for signs of infection, such as redness, swelling, severe pain, or unusual discharge, and inform the doctor if these appear. Additionally, maintaining proper wound hygiene, changing dressings as recommended, and avoiding factors that may worsen the situation, such as constant pressure on the wound or smoking, is essential.
Diagnosing non-healing wounds involves several steps and assessments to identify the underlying causes and determine the best treatment plan.
First, the doctor will take a detailed medical history of the patient, including pre-existing conditions such as diabetes, vascular diseases, autoimmune disorders, or other health issues that could contribute to delayed wound healing. This also includes reviewing the medications the patient is taking, as some medications can negatively affect the healing process.
Physical examination of the wound is essential. The doctor will assess the size, depth, location, and appearance of the wound, as well as the presence of any signs of infection, such as redness, swelling, or abnormal discharge. Based on the wound's appearance, additional tests may be performed.
Common lab tests include bacterial culture analysis to identify possible infections, as well as blood tests to assess glucose levels, kidney function, and other parameters that could influence healing. Imaging tests, such as Doppler ultrasounds or angiographies, may be used to assess blood circulation in the affected area, especially if vascular disease is suspected.
In some cases, a tissue biopsy from the wound area may be necessary to rule out the possibility of a more serious condition, such as skin cancer or other chronic skin diseases.
Based on these evaluations, the doctor will be able to identify the cause of delayed healing and recommend appropriate treatment, which may include both local measures (cleaning and wound care) and systemic treatments to address underlying problems.
What are the treatments for non-healing wounds?
When we talk about wounds that "do not heal," we refer to the fact that these wounds do not heal normally, without additional interventions, within a timeframe that would be considered typical for other similar wounds. Usually, a wound should start to heal and close within a few weeks. If this does not happen, the wound is considered chronic or improperly treated.
The essential issue with these wounds is that they do not heal on their own due to factors such as poor blood circulation, persistent infections, uncontrolled diabetes, malnutrition, or other medical conditions. These factors prevent the body from following the normal healing process. However, the fact that these wounds do not heal on their own does not mean they cannot be treated. There are numerous available treatments that can stimulate and support the healing process, but the main problem is that without these interventions, the wound would not tend to heal on its own in a normal and predictable manner. The treatments below are essential to overcoming the obstacles that hinder healing and helping the wound close and fully regenerate.
1. Cleaning and Debridement of Non-Healing Wounds
The first essential step in the treatment of a chronic wound is proper cleaning to remove dead tissue, debris, and bacteria that may hinder healing. This process, called debridement, can be performed
mechanically, surgically, enzymatically, or with the help of specialized dressings. The goal is to create a clean environment conducive to the regeneration of healthy tissues.
The debridement process and the treatment of chronic wounds are usually managed by a multidisciplinary team of specialized physicians. This may include dermatologists, who specialize in skin
conditions, vascular surgeons, who address improving circulation when it is compromised, and doctors specialized in diabetology, especially if the wound is related to complications of diabetes.
After debridement, the wound will be closely monitored for any signs of infection or progress in healing. The physician will establish a care plan that may include periodic dressing changes,
application of local treatments such as antimicrobial ointments, and may recommend additional therapies, such as hyperbaric oxygen therapy, if necessary.
During this process, the patient will also
be evaluated for any underlying conditions that may hinder healing, such as uncontrolled diabetes or vascular diseases. Based on these evaluations, adjustments to the treatment may be necessary, such as
changing the medication regimen or recommendations for lifestyle improvements to support the healing process. The goal is to treat not only the wound itself but also to address all factors contributing to its
chronicity.
2. Application of Special Dressings on Non-Healing Wounds
Special dressings play a crucial role in the treatment of non-healing wounds, as they are designed to create an optimal healing environment. The correct choice of dressing depends on the type of wound, the
amount of exudate (drainage), and the stage of healing.
One type of dressing is the hydrocolloid dressing, which forms a gel upon contact with the wound exudate, thus keeping the wound moist and reducing pain during dressing changes. These are suitable
for wounds with a moderate amount of drainage. In cases where the wound is dry or has necrotic tissue, hydrogel dressings are used, which help to hydrate the wound and remove dead tissue, creating a favorable
environment for tissue regeneration.
For wounds that produce a large amount of drainage, foam dressings are an effective choice. They absorb excess exudate, keeping the wound clean and protecting
the surrounding skin from maceration. These dressings also provide a barrier against bacteria. In cases where there is a risk of infection or the wound is already infected, dressings impregnated with silver are
often used due to their antimicrobial properties. Additionally, alginate dressings, made from seaweed, are highly absorbent and useful for wounds with abundant drainage.
The application and change
of special dressings must follow a strict schedule established by the physician. Changing too frequently can disrupt healing, while changing too rarely can lead to the accumulation of drainage and increased
risk of infection. Before applying a new dressing, the wound must be carefully cleaned to remove any accumulated debris or exudate. Careful assessment of the wound at each change is crucial to monitor the
progress of healing and to adjust the treatment if necessary.
3. Infection Control

If the wound is infected, treatment will include the use of antibiotics, either orally or applied locally, to combat the bacteria. Identifying the specific bacteria causing the infection is crucial for
selecting the appropriate antibiotic treatment. This is done by taking cultures from the wound and performing an antibiogram. This test helps determine the sensitivity of the bacteria to different antibiotics,
allowing the physician to select the most effective treatment.
In addition to antibiotic treatments, it is essential to maintain a clean and protected environment at the wound site. This is achieved by using appropriate dressings, which not only protect the
wound from external contamination but may also contain antimicrobial substances to actively combat infections.
Patients should be very attentive to signs of infection, such as redness, swelling,
localized warmth, increased pain, or the presence of pus. If these symptoms occur, it is important to contact the physician immediately to adjust the treatment.
In some cases, severe infections may
require surgical interventions to remove infected tissues and prevent the spread of infection. Additionally, in extreme situations, hospitalization may be necessary for more intensive treatments, such as
intravenous antibiotic therapy or extensive surgical interventions.
The patient and their caregivers should receive detailed instructions from the attending physician, whether it is a dermatologist,
surgeon, or wound care specialist, regarding the application and changing of dressings to minimize the risk of infection and ensure optimal healing. In some cases, dressing changes may be performed at home, but
it is essential to strictly follow the physician’s recommendations to avoid complications.
4. Hyperbaric Oxygen Therapy and Improving Blood Circulation
Treatment of non-healing wounds often requires interventions to improve blood circulation and provide additional oxygen to the affected tissues. Adequate blood circulation is essential for wound healing, as
blood carries the oxygen and nutrients necessary for cell regeneration and removes metabolic waste from the affected area.
To improve blood circulation in areas with chronic wounds, several methods and interventions can be used. One of the most common approaches is moderate physical exercise, which can stimulate blood
flow, especially in the extremities. For example, walking or stretching exercises can help improve circulation in the legs, where chronic wounds are common, especially in people with diabetes.
Another frequently used treatment is compression therapy, which involves the use of compression stockings or bandages. These devices apply pressure to the limbs, helping to increase venous blood
flow and reduce edema, a factor that can worsen chronic wounds.

Hyperbaric oxygen therapy is an advanced treatment method that can be extremely effective for wounds that do not heal, especially when it comes to wounds complicated by poor circulation. This therapy
involves placing the patient in a special chamber where the ambient pressure is greater than normal atmospheric pressure. In this environment, the patient breathes pure oxygen, usually through a mask.
Thus, the amount of oxygen dissolved in the blood significantly increases, allowing oxygen to penetrate deeper into the affected tissues, even in areas where blood circulation is compromised. The
increase in oxygen levels in tissues stimulates healing processes, reduces inflammation, and combats infections by strengthening the body's immune response.
Hyperbaric oxygen therapy is particularly
useful in treating a wide range of wounds and chronic conditions that do not respond to conventional treatments. This includes, in particular, diabetic ulcers, which are open wounds that occur on the feet of
people with diabetes. These wounds are often difficult to heal due to poor circulation and neuropathy, and hyperbaric oxygen therapy can significantly accelerate the healing process by improving oxygenation of
the affected tissues. A study conducted in 2018 found that hyperbaric oxygen therapy was effective in treating 74.2% of cases of diabetic-related ulcers. The use of hyperbaric therapy significantly improved the
healing process of ulcerative lesions compared to other treatment methods.
Another specific example is the treatment of radiation-induced wounds. After radiation therapy, patients may develop
chronic wounds or necrosis (tissue death) in the treated areas. These wounds are often resistant to healing due to damage to blood vessels and tissues. Hyperbaric oxygen therapy helps regenerate damaged tissue
and create new blood vessels, a process known as angiogenesis, which is essential for restoring normal tissue function.
Hyperbaric oxygen therapy is also beneficial in treating chronic
osteomyelitis, a severe bone infection that can occur as a result of open wounds or surgical interventions. In these cases, the therapy helps destroy anaerobic bacteria and stimulates the healing process of the
bone and surrounding tissues.
Gas gangrene, a rare but extremely dangerous infection caused by bacteria that thrive in the absence of oxygen, can be effectively treated with hyperbaric oxygen
therapy. In this case, the therapy increases the oxygen concentration in tissues to levels that are toxic to anaerobic bacteria, thus helping control the infection and preventing its spread.
Hyperbaric oxygen therapy is also used in cases of severe trauma, such as crush injuries, where blood flow to tissues is compromised, leading to ischemia (lack of oxygen) and tissue death. The
therapy can help reduce inflammation, limit the spread of necrosis, and stimulate regeneration processes.
Another application area is in the treatment of severe burns, where therapy can help reduce
edema, prevent infections, and accelerate healing by stimulating the regeneration of skin and underlying tissues.
To benefit from hyperbaric oxygen therapy, it is important to seek specialized and
licensed medical centers where the treatment is administered by qualified medical personnel. These centers utilize advanced equipment and follow strict protocols to ensure the safety and efficacy of the
treatment.

In Romania, Hyperbarium is one of the most advanced and modern hyperbaric medicine clinics. Located near Băile Felix, the Hyperbarium clinic offers access to state-of-the-art hyperbaric equipment specifically
designed for treating non-healing wounds and other conditions that require oxygen therapy. Each patient is individually evaluated to establish a personalized treatment plan tailored to their specific needs,
thus ensuring the effectiveness and safety of the therapy. The entire clinic staff is trained and certified according to European standards, guaranteeing the highest therapy standards. The doctors at the clinic
have expertise in hyperbaric medicine, in accordance with the Order of the Minister of Health No. 418/2005, and apply treatment protocols approved and regulated by the European Committee of Hyperbaric Medicine
(ECMH).
The medical director of the clinic, Dr. Ciprian Sturz, is a surgeon specialized in general surgery, visceral surgery, and emergency surgery, bringing extensive expertise in managing and treating
complex wounds. Moreover, the clinic has an integrated telemedicine system that allows real-time monitoring of hyperbaric treatment by specialist doctors from international centers of medical excellence, thus
ensuring the highest quality care. Read more about how hyperbaric therapy works or schedule a consultation to discover how this
therapy can be the right solution for you.
It is essential to be aware that there are unauthorized hyperbaric chambers on the market, which can pose significant risks. These chambers, often operated
outside of proper medical supervision, do not meet the necessary safety standards and can lead to serious complications. The use of such chambers can cause adverse effects, such as ear injuries, lung damage, or
even oxygen toxicity if the therapy is not administered correctly. Therefore, it is crucial to choose an authorized center to avoid these risks and to benefit from all the advantages that hyperbaric oxygen
therapy can offer.
5. Use of Growth Factor Therapy
Growth factor therapy represents another innovative approach in the treatment of wounds that do not heal. This method involves the use of natural proteins known as growth factors, which play a crucial role in
tissue regeneration and healing processes. Growth factors are naturally present in the body and are responsible for stimulating cell proliferation, forming new blood vessels (angiogenesis), and accelerating
tissue repair.
In this therapy, growth factors can be applied directly to the affected wound, either in the form of gels or creams, or through injection. They can be derived from the patient's blood through a
procedure known as "platelet-rich plasma" (PRP), where blood is processed to concentrate the platelets, the cells that contain a large amount of growth factors. This platelet concentrate is then applied
directly to the wound to stimulate healing.
Growth factors accelerate the healing process by attracting essential cells to the wound site, such as fibroblasts and keratinocytes, which contribute to
the formation of new tissues. They also help create new blood vessels, which are essential for supplying oxygen and nutrients to the affected area, which is especially important in chronic wounds where blood
circulation is compromised.
One of the main benefits of growth factor therapy is its ability to reduce healing time while improving the patient's quality of life. Additionally, using the patient’s own growth factors (through PRP)
minimizes the risk of adverse reactions or rejection since the biological material is autologous, meaning it comes from the patient’s body.
Growth factor therapy is conducted under the strict
supervision of physicians specialized in dermatology, vascular surgery, and plastic surgery, who have experience in treating chronic wounds. After applying the therapy, the wound is closely monitored by these
specialists to assess healing progress and adjust treatment based on the individual patient's response. In some cases, multiple treatment sessions may be necessary to achieve the desired results.
6. Surgical Interventions
If the wound does not respond to other forms of treatment, surgical intervention may be necessary. This may include skin grafts, which involve transplanting healthy skin from another part of the body, or even more complex interventions to repair affected tissues and blood vessels.
Complications That May Arise in Non-Healing Wounds
Non-healing wounds, also known as chronic wounds, can lead to a series of serious complications if not managed and treated properly. These complications not only worsen the overall health of the patient but can also be life-threatening in some cases. Here are some of the most common and dangerous complications associated with non-healing wounds:
- Severe infections: One of the most common complications is bacterial infection, which can be superficial or deep. If the infection spreads to the deep tissues or into the blood, it can lead to sepsis, a life-threatening condition that requires emergency medical treatment. Untreated infections can also lead to osteomyelitis, a bone infection that is difficult to treat and often requires surgical intervention.
- Amputation: In severe cases, especially in patients with diabetes or peripheral vascular diseases, chronic wounds can lead to gangrene, which is the death of tissue due to lack of circulation. If gangrene is not treated in time, the only option often remains amputation of the affected limbs to prevent the spread of infection and to save the patient's life.
- Excessive scarring and contractures: Wounds that heal slowly or incompletely can lead to excessive scarring or the formation of thick scar tissue, also known as keloid. This tissue can affect the mobility and functionality of the affected area, causing contractures—a complication in which the skin and underlying tissues tighten, limiting movement.
- Chronic pain: Chronic wounds can be accompanied by persistent pain, which can significantly affect the patient's quality of life. Chronic pain can lead to additional problems, such as sleep disorders, depression, and anxiety.
- Increased cancer risk: Although rare, there is a risk that a chronic wound, especially one that lasts for years, can evolve into a form of skin cancer, such as squamous cell carcinoma. This occurs when the cells in the affected area undergo abnormal changes due to chronic inflammation and constant exposure to irritants.
- Social isolation and psychological impact: Patients with chronic wounds often face significant psychological impact. The appearance of the wound, constant pain, and physical limitations can lead to social isolation, depression, and anxiety. This can worsen the patient's overall health and reduce their ability to follow necessary treatments.
- Cardiovascular complications: Chronic inflammation associated with non-healing wounds can contribute to the worsening of pre-existing cardiovascular diseases. For example, patients with chronic wounds and diabetes have an increased risk of major cardiovascular events, such as heart attacks or strokes.
- Kidney complications: Patients with chronic wounds, especially those with diabetes, are more prone to developing kidney complications, such as chronic kidney failure. This can be aggravated by the prolonged use of certain medications or significant losses of proteins and other nutrients through wound exudate.
- Systemic complications: Chronic wounds can have effects on the entire body, not just on the affected area. They can lead to systemic inflammatory states, which contribute to the deterioration of other organs, and can worsen pre-existing diseases, such as cardiovascular diseases.
Prevention methods for non-healing wounds
Preventing non-healing wounds is essential for maintaining health and avoiding serious complications. To prevent the occurrence of these wounds, especially in high-risk individuals, such as patients with
diabetes or vascular diseases, there are several effective methods.
Maintaining proper skin hygiene is an important first step. It is essential to keep the skin clean and dry to prevent infections and the occurrence of wounds. Using gentle skin care products
that do not irritate the skin helps maintain the natural barrier of the skin intact, especially in areas prone to friction or pressure, such as the feet and elbows.
Proper management of chronic diseases,
such as diabetes and vascular diseases, is vital. Strict control of blood sugar in diabetic patients and maintaining blood pressure and cholesterol within normal limits are essential measures for preventing
wounds. Additionally, diabetic patients should pay special attention to foot care, examining them daily to identify any injuries or pressure points and wearing appropriate footwear that reduces the risk of
ulcers.
Another aspect is close monitoring of immobilized patients. In the case of patients with reduced mobility, it is essential not only to frequently change positions but also to use
mattresses and cushions specifically designed to reduce pressure on vulnerable areas of the body. These devices help evenly distribute weight and reduce the risk of pressure sores.
Monitoring nutritional status
is also crucial. Patients suffering from malnutrition or those with deficiencies in vitamins and minerals are more prone to developing chronic wounds. Supplementing the diet with necessary nutrients can help
maintain skin integrity and promote healing in case of injuries.
Using protective equipment at work is essential for preventing injuries, especially in industries where there is an increased
risk of accidents or exposure to hazardous substances. Ensuring safe working conditions and proper equipment can prevent injuries that, in the absence of proper treatment, can become chronic.
Managing stress
can play an important role in preventing chronic wounds. Chronic stress can negatively affect the immune system and hinder the proper healing of wounds. Through relaxation techniques, therapy, and activities
that reduce stress, the body’s response to injuries can be improved.
Finally, regular consultations with a specialist doctor, especially for individuals with chronic conditions or a history
of wounds that have not healed properly, are vital. The doctor can identify risk factors, recommend appropriate preventive measures, and monitor the overall health of the skin, intervening promptly if needed.
In conclusion, difficult-to-heal wounds are not only a physical challenge but also a signal that the body needs special attention. Whether due to internal factors such as pre-existing health issues,
infections, or inadequate care, prolonging the healing process can be frustrating and risky. However, with the right treatments and careful care, even the most difficult wounds can return to the healing path.
Listening to medical recommendations, maintaining strict hygiene, and constant monitoring are key to preventing complications and supporting faster recovery, restoring comfort and health to us.




