
Article reviewed by: Dr. Sturz Ciprian, Dr. Tîlvescu Cătălin and Dr. Alina Vasile
Article updated on: 11-12-2024
All About Burns: Types, Treatments and Recovery
- What are burns?
- What are the main causes of burns?
- What are the types of burns based on severity?
- What are the types of burns based on cause?
- What are the symptoms of burns?
- How are burns diagnosed?
- What is first aid for burns?
- What are the treatments for burns?
- Complications of burns
- Methods for preventing burns
- Frequently asked questions and myths about burns
What are burns?
Burns are injuries to the skin and deep tissues caused by contact with heat, chemicals, electricity, radiation, or friction. Depending on severity, they can affect only the superficial layer of the skin or can destroy deeper structures, including blood vessels, nerves, muscles, and bones. The severity depends on both the depth of the injury and the affected body surface area. Burns can cause redness, pain, blisters, and in severe cases, loss of sensation, risk of infection, dehydration, shock, and impairment of internal organ functions. In the long term, they can lead to scarring, loss of skin elasticity, and the need for reconstructive surgical interventions.
Worldwide, burns represent the fourth leading cause of death from traumatic injuries, causing approximately 330,000 deaths annually. A study published in the Romanian Medical Journal shows that burns, regardless of their cause, represent one of the most frequent types of accidents in children, with no notable differences between sexes.
Main causes of burns:
Burns occur from multiple causes, but the most common are:
- Fire – Flames from fires, stoves, or candles can cause severe burns.
- Liquids and steam – Boiling water, hot coffee, or steam can burn the skin quickly.
- Hot objects – Irons, hot pans, or engines can cause burns through contact.
- Chemicals – Acids, caustic soda, and cleaning products can cause severe burns.
- Electricity – Exposed wires or defective equipment can cause severe burns.
- Sun – UV radiation can burn the skin and increase the risk of cancer.
- Friction – Falls on asphalt or tight clothing can cause burns, also known as "friction burns."
- Explosions – Gases or fireworks can lead to severe burns.
- Hot water in the bath – Showers or baths that are too hot can cause serious burns, especially in children.
- Flammable substances – Gasoline or alcohol can catch fire on skin.
What are the types of burns based on severity?
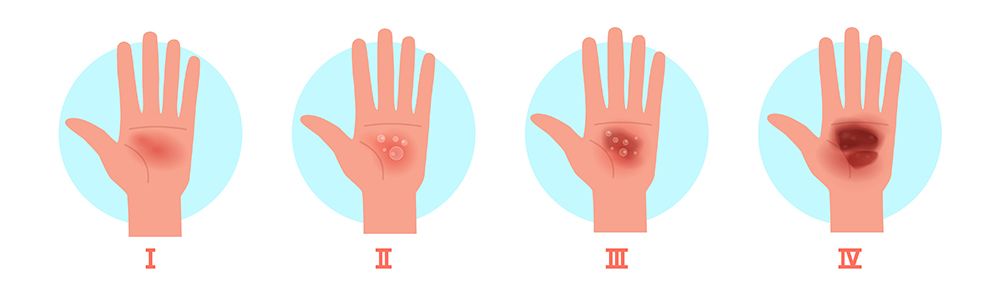
First-Degree (Superficial) - First-degree burns are the most superficial types of burns, affecting only the upper layer of the skin (epidermis). They do not cause permanent damage and heal quickly, usually without scarring. Although they can be painful, they are not normally dangerous and do not require medical assistance, except in special cases (extensive burns or in vulnerable people, such as children and the elderly). These burns do not cause blisters, but can lead to skin peeling after a few days. Although they are mild, they can be uncomfortable and can increase skin sensitivity to sun and other irritations. The most common example of a first-degree burn is sunburn, which occurs when the skin is exposed too much to ultraviolet rays without adequate protection.
Second-Degree (Partial thickness) - Second-degree burns are deeper than first-degree burns because they affect both the epidermis and the superficial layer of the dermis. These burns can cause severe discomfort and have a higher risk of complications, such as infections or scarring. Unlike superficial burns, these require more time to heal and can leave marks on the skin. A distinctive element of second-degree burns is the formation of fluid-filled blisters, which appear due to damage to the protective layer of the skin. These should not be broken, as they can increase the risk of infection and can slow down the healing process. Recovery time varies depending on the severity of the burn. If only part of the dermis is affected, the skin can regenerate in 10-14 days, with minimal risks of scarring. If the burn is deeper, healing can take several weeks, and the newly formed skin may have a different color than the original. In some cases, when the burned surface is extensive or located in sensitive areas (face, hands, feet, genitals), medical consultation may be necessary to avoid complications. If the burn does not heal in a timely manner or shows signs of infection (pus, unpleasant odor, fever), medical intervention becomes necessary.
Third-Degree (Full thickness) - Third-degree burns are extremely serious because they destroy all layers of the skin, including the epidermis and dermis, and can reach deeper tissues, such as muscles and nerves. Unlike more superficial burns, they affect the essential structures of the skin, which makes natural healing very difficult and often impossible without medical intervention. A distinctive sign of these burns is the loss of sensitivity in the affected area, as the nerve endings are destroyed. The skin may have a whitish, brown, black, or charred appearance, and its texture becomes rigid and dry. These injuries do not form blisters, as the layers of the skin are completely damaged. In most cases, treatment involves intensive medical care, and skin grafts are often necessary to help repair the affected area. Without proper treatment, these burns present a high risk of severe infections, dehydration, and life-threatening complications. These burns usually occur after prolonged exposure to flames, contact with aggressive chemicals, electrocutions, or direct contact with extremely hot liquids. Anyone who suffers a third-degree burn must receive immediate medical assistance, as recovery is a complex and long-term process.
Fourth-Degree - Fourth-degree burns are more severe than third-degree burns because they completely destroy the skin and affect deep tissues, including muscles, tendons, and even bones. Unlike third-degree burns, where skin is still present, albeit damaged, in the case of fourth-degree burns, tissues can be completely destroyed or charred. A distinctive sign of these burns is the exposure of internal structures, such as muscles, subcutaneous fat, or even bone, which makes them extremely dangerous. The affected skin may have a charred, gray, or whitish appearance, and the dead (necrotic) tissues no longer have any regeneration capacity. Unlike less severe burns, these injuries not only affect the mobility and functionality of the affected area but endanger life through the high risk of infections and systemic complications. Natural healing is impossible, and treatment almost always involves removing dead tissues through surgical intervention. In many cases, amputation of severely affected areas or complex reconstruction procedures with skin grafts and tissue transplants is necessary. Without urgent medical treatment, these burns can quickly lead to severe infections, septic shock, and multiple organ failure. Such burns occur as a result of extreme events, such as prolonged fires, severe electrocutions, explosions, or direct exposure to extremely corrosive substances.
In addition to first, second, third, and fourth-degree burns, there are also fifth and sixth-degree burns, but these are extremely rare and usually lethal. The most common are first and second-degree burns, which occur in everyday life and can be treated at home or with minimal medical help. Third-degree burns are rarer and occur in serious accidents, such as fires, prolonged contact with hot liquids, or electrocutions. Fourth-degree burns are even more severe and occur in extreme situations, such as industrial accidents or prolonged exposure to intense flames. Fifth and sixth-degree burns have an extremely reserved prognosis, and chances of survival are minimal even with intensive medical treatment.
What are the types of burns based on cause?
-
Thermal burns are the most common types of burns and occur when the skin comes into contact with a heat source intense enough to cause injury. Their severity varies depending on the duration of
exposure, the temperature of the source, and the affected surface. An important aspect of thermal burns is that they can continue to affect tissues even after the heat source is removed. For example, if a
person spills a hot liquid on the skin, it can remain on the surface and continue to produce injuries until it is removed. The same applies to clothes that have caught fire or hot objects that remain stuck
to the skin.
An essential characteristic of thermal burns is the risk of infection, especially in cases where the skin is destroyed and can no longer protect the affected area. In these situations, exposure to bacteria from the environment can lead to serious complications, and proper care becomes essential for their prevention. Common examples of thermal burns include those caused by contact with hot liquids, such as coffee spilled on the skin, accidental contact with hot objects, such as an iron or stove plate, and exposure to flames, as happens in house fires. Other situations include burns caused by hot vapors, such as those that occur when opening the lid of a pressure vessel, or contact with hot metals, such as hot pipes or parts of a car engine. Thermal burns can range from minor injuries to critical conditions, and their severity depends on the speed of intervention and the measures taken immediately after the incident. -
Chemical burns are caused by contact of the skin, eyes, or internal tissues with aggressive substances that can destroy cells and affect the chemical balance of the body. Unlike thermal burns, which
are triggered by high temperatures, chemical burns do not depend on heat, but on the reaction between the substance and the body structures. These burns can be caused by both acids and strong bases, which
tend to penetrate tissues deeper than surface burns.
One aspect that makes them dangerous is the fact that tissue damage can continue even after the apparent removal of the substance, especially if it has been absorbed into the skin or has entered the bloodstream. Some chemicals, such as sodium hydroxide or hydrofluoric acid, can cause extensive destruction without immediately causing a strong sensation of pain, which can delay the reaction of the affected person. In some cases, a chemical burn does not initially appear serious, but its effects become evident after a few hours.
The situations in which these burns occur are diverse. Chemicals in household cleaning products, such as bleaches or drain cleaning solutions, can cause serious injuries if not handled correctly. In industry, workers who come into contact with concentrated acids, caustic bases, or toxic solvents are exposed to the risk of severe chemical burns. In laboratories, substances such as silver nitrate or high-concentration hydrogen peroxide can cause dangerous injuries if mishandled.
The impact of a chemical burn depends on the speed of reaction and the measures taken to neutralize the substance. If not treated properly, such a burn can lead to permanent scars or internal complications that require long-term medical interventions. -
Electrical burns occur when the body comes into contact with a source of electricity, causing injuries to the skin and internal tissues. Unlike other types of burns, these can affect both the body
surface and deep structures, as electricity moves through the body, generating heat and destroying cells from the inside. In some cases, internal injuries can be much more serious than those visible on the
outside, and effects can include cardiac arrest, nerve damage, or failure of organs affected by the current.
The severity of an electrical burn depends on factors such as electrical voltage, duration of contact, and the path of the current through the body. Exposure to low voltages, such as those in the household, can cause superficial burns, but can also lead to muscle contractions that prolong contact with the electrical source. On the other hand, high-voltage electrocutions, as encountered in industrial accidents or high-voltage lines, can cause serious injuries, including carbonization and destruction of internal organs.
Although an electrical burn may seem minor on the surface, internal damage can continue even after contact with the current source is interrupted. In many cases, affected people may present delayed symptoms, such as cardiac or neurological problems, which makes a medical evaluation necessary even when external injuries seem insignificant. -
Radiation burns occur when the skin or internal tissues are exposed to a source of ionizing or non-ionizing radiation for a period long enough to cause cellular injury. Unlike thermal or chemical
burns, these are not caused by direct contact with a hot or corrosive substance, but by the effects of radiation on cells, which can lead to inflammation, cell death, and, in severe cases, genetic changes
that increase the risk of cancer.

Sunburns are the most common examples, being caused by ultraviolet radiation emitted by the sun or artificial sources, such as tanning lamps. Exposure to ionizing radiation, such as that used in radiotherapy or in nuclear accidents, can cause deeper injuries, affecting both the skin and internal organs. In such cases, tissue damage can continue even after exposure stops, and recovery can be difficult, especially if essential body structures have been affected.
The effects of a radiation burn can range from mild redness and peeling, as in the case of sunburns, to severe necrosis and systemic deterioration in the case of strong exposures. Although some injuries may be reversible, repeated or intense exposure can lead to long-term complications, which is why adequate protection and limiting exposure are essential for prevention.
What are the symptoms of burns?
The symptoms of burns vary depending on severity, but in general, any burn causes visible discomfort. The mildest burns cause redness and pain, while the most severe can lead to complete destruction of the skin and even the tissues underneath.
In the case of mild burns, such as sunburns or those from a quick touch of a hot object, the skin becomes red, sensitive, and may begin to peel after a few days. Usually, these are only superficial and heal on their own without problems. If the burn is deeper, fluid-filled blisters may appear, which are a sign that the skin has suffered more serious damage. These blisters are fragile and, if broken, can expose the sensitive skin underneath, increasing the risk of infection.
When the burn is very severe, pain can be paradoxically absent, because the nerve endings in the skin are destroyed. The affected skin may have a whitish, brownish, or charred appearance, and in some cases, may appear dry and hard to the touch. If the burn has also affected the deep layers of the skin, the area may be completely without sensation. In such situations, the injuries do not heal on their own and require medical care, as there is a risk of serious complications, such as severe infections or loss of functionality in the affected area.
In the case of burns caused by chemicals or electricity, symptoms may also appear inside the body, not just on the surface. A person who has suffered an electrical burn, for example, may have only a small mark on the skin, but may have suffered serious internal injuries along the path of the current through the body. Similarly, exposure to chemicals can cause burns that continue to worsen even after the skin has been washed.
If a burn is extensive, meaning it affects a large area of the body, the person may present additional symptoms such as dizziness, nausea, or even loss of consciousness due to pain and fluid loss. In such cases, immediate medical help is needed to avoid complications.
How are burns diagnosed?
Burns are diagnosed mainly through visual examination of the skin and through evaluation of symptoms. A doctor will analyze how extensive the burn is, how deeply it has penetrated the skin, and if there are signs of complications, such as infections or damage to deeper tissues.
How do you differentiate between a superficial burn and a severe one?
The difference between a superficial burn and a severe one can be observed based on pain, skin appearance, and how deeply the tissue is affected.
A superficial burn affects only the outer layer of the skin. Usually, the skin becomes red, is warm to the touch, and causes a stinging sensation or mild pain. A common example is sunburn or a quick touch of a hot object, such as a hot pan. If the burn is a bit deeper, fluid-filled blisters may appear, which indicates a more serious injury, but one that still has a high chance of healing without scarring.
A severe burn penetrates deeper into the skin and can affect even the tissues underneath. If the skin takes on a whitish, brownish, or even charred color, and the affected area does not hurt, it is a sign that the nerves have been destroyed and the burn is severe. In these cases, there is an increased risk of infection, fluid loss, and other complications, which means that emergency medical care is needed.
When should you see a doctor?
A simple way to determine how serious a burn is is to pay attention to pain. If the burn is extremely painful, it is most likely a superficial one, which means that the nerves in the skin are still functional and sending signals to the brain. For example, if you got sunburned or touched a hot pan for a fraction of a second, you will feel an intense stinging, but the skin will remain intact or, in more serious cases, will develop blisters. These burns usually heal without problems, with proper care.
On the other hand, if the burn is very extensive or very deep and does not hurt at all, this can be a sign of extreme severity. The absence of pain occurs when the burn has completely destroyed the nerve endings, which means that the skin and tissues underneath are severely affected. Such a situation is dangerous, as the affected person may believe that the burn is not that serious due to the lack of pain, but, in reality, it may be a severe injury that requires urgent medical intervention.
Another important aspect is the size and location of the burn. If the burn covers a large area of the body, even if it seems superficial, it can lead to the loss of a significant amount of fluids, which can cause dehydration and shock. In addition, some areas are much more sensitive and exposed to the risk of complications. For example, burns on the face, hands, feet, genitals, or joints can affect long-term functionality and have a higher risk of severe scarring. In these cases, medical consultation is necessary to prevent complications.
Also, attention should be paid to signs of infection, especially if the burn does not heal or the affected area begins to look different over time. If symptoms such as extensive redness, swelling, pus, unpleasant odor, fever, or chills appear, these indicate a possible infection that can spread bacteria into the blood, leading to serious complications. In such situations, it is important to see a doctor for appropriate treatment, as an untreated infection can lead to serious health problems.
In short, you should see a doctor immediately if the burn does not hurt at all, is very extensive, affects sensitive areas, or shows signs of infection. In milder cases, burns can be treated at home, but if there are doubts about their severity, the safest is to ask for a specialist's opinion.
What does the doctor do to diagnose the burn?
-
Visual examination of the skin:
The first thing the doctor does is analyze the color of the skin and the appearance of the burned area. A superficial burn is red and moist, while a more serious one may have blisters or even a dry, whitish, or charred surface, indicating destruction of the deep layers of the skin. The doctor also checks if the skin is still elastic or if it has become rigid and necrotic, which may indicate a severe burn. -
Evaluation of pain and sensitivity:
A simple test that the doctor can do is to lightly touch the affected area or use a soft object to check if the patient feels the touch. If the burn is superficial, the pain is intense, but if it is deep and the patient no longer feels anything, it is a sign that the nerve endings have been destroyed. -
Determining the size of the burn:
The doctor estimates the affected surface using the Rule of 9% (a method used to calculate the percentage of the body burned). This rule divides the body into regions (head, arms, chest, abdomen, legs), each having a percentage of the total skin surface. If the burn exceeds a certain percentage, it can be considered critical and requires special care. -
Checking systemic symptoms
If the burn is large or deep, the doctor checks for signs of dehydration, shock, or infection. For example, an accelerated pulse, low blood pressure, or fever may indicate a serious complication. If the patient has been exposed to smoke or toxic gases, the doctor will also check the breathing to ensure there are no injuries to the airways. -
Additional tests (if necessary):
If the burn is severe, the doctor may recommend blood tests to check the electrolyte balance and the risk of infection. In the case of an electrical burn, an electrocardiogram may be necessary to check if the heart has been affected by the current. If there is suspicion of an internal burn (for example, through inhalation of smoke or toxic substances), x-rays or lung function tests may be done.
Based on these evaluations, the doctor decides whether the burn can be treated at home, requires advanced medical care, or even surgical interventions, such as skin grafts.
What is first aid?

First aid for burns should be applied quickly to limit skin damage and prevent complications. The correct mode of intervention depends on the severity of the burn, but there are some general measures that can be followed for any type of burn.
-
Removing the burn source
If the person is still in contact with what caused the burn, the first step is to safely remove them from the dangerous source. In the case of burns caused by fire, flaming clothes should be extinguished by rolling the victim on the ground or by covering with a blanket. For chemical burns, it is essential to quickly remove the dangerous substance, rinsing the area with plenty of water. -
Cooling the affected area
For mild or moderate burns, the affected area should be kept under cold water (not ice!) for 10-15 minutes. This reduces the temperature of the skin, alleviates pain, and prevents the burn from spreading in depth. If you don't have access to a tap, you can use wet and cold compresses. -
Protecting the skin
If the burn is superficial, it can be covered with a sterile dressing, gauze, or a clean material, to prevent contact with bacteria. Butter, oil, toothpaste, or other home remedies should not be applied, as they can worsen the situation or increase the risk of infection. -
Avoiding breaking blisters
Blisters usually appear after a period, not immediately at the time of the burn. However, in some cases, especially in second-degree burns caused by hot liquids or chemicals, blisters can form quite quickly. Therefore, avoiding breaking them is an important measure in subsequent care, but can also be included in first aid if blisters are already present at the time of intervention. If blisters appear, they should be left intact, as they act as a natural barrier against infections. If they accidentally break, the exposed skin should be gently cleaned and covered with a sterile dressing. -
Administering a painkiller, if necessary
For pain, an anti-inflammatory medication, such as ibuprofen, can be taken. This helps reduce inflammation and discomfort.
Rapid and correct intervention can make the difference between healing without complications and a burn that worsens or leaves permanent scars.
What are the treatments for burns?
Treatments for burns vary depending on the severity of the injury and the affected area. Some minor burns can be treated at home, while others require specialized medical care.
Treatment for mild burns (first-degree and some second-degree)

For superficial burns, the main treatment consists of relieving pain, protecting the skin, and preventing infections. After cooling the affected area with cold water for 10-15 minutes, a soothing gel with aloe vera or a moisturizing lotion can be applied to keep the skin moist and prevent peeling. If the burn causes discomfort, painkillers such as ibuprofen or paracetamol can be administered.
If blisters appear, they should not be broken, as they serve as a natural barrier against infections. The area can be covered with a sterile, non-adhesive dressing, and the skin should be protected from sun exposure and irritation. In a few days, the burn heals on its own, and the affected skin may begin to peel.
Treatment for larger and more severe burns (deep second-degree and third-degree)

In the case of deeper burns, treatment should be carried out under medical supervision to prevent infections, fluid loss, and further tissue damage. Antibiotic ointments, such as Silver Sulfadiazine, are used for skin protection, and patients with extensive burns may need intravenous fluids to prevent dehydration and shock.
A treatment increasingly used in recent years, due to proven benefits in accelerating healing, is hyperbaric therapy. This involves placing the patient in a hyperbaric chamber, where they breathe pure oxygen at a pressure higher than atmospheric. This method is extremely effective because oxygen reaches deeper into the affected tissues, helping skin regeneration and reducing the risk of necrosis.
Why is hyperbaric therapy so important now?

The importance of hyperbaric therapy has recently increased, especially due to advances in regenerative medicine and recognition of the role of hyperbaric oxygen in fighting infections and accelerating cellular repair. In the case of extensive burns, this method can prevent serious complications, such as systemic infections and the need for amputation, helping to form new blood vessels in affected areas. Recent studies have shown that this method reduces inflammation, stimulates tissue repair, and significantly decreases the risk of infections, one of the main complications of severe burns.
Another extremely important aspect is the impact on patients with extensive burns, where lack of oxygen in tissues can quickly lead to cell death and serious complications. Through intensive oxygenation, hyperbaric therapy helps:
- Improve blood flow in burned areas, preventing necrosis and saving as much viable tissue as possible.
- Stimulate the formation of new blood vessels (angiogenesis), accelerating skin regeneration.
- Increase the survival rate of patients with severe burns, especially those admitted to major burn centers.
Another major benefit is its role in preventing severe infections, which represent one of the biggest threats to patients with extensive burns. Bacteria that cause serious infections, such as Pseudomonas aeruginosa or Staphylococcus aureus, develop more slowly in oxygen-rich environments, which means that hyperbaric therapy also has a powerful antimicrobial effect.
In the context of burns caused by fires, many patients suffer not only from skin burns but also from carbon monoxide and cyanide poisoning, inhaled from thick smoke. These substances drastically reduce the blood's ability to transport oxygen, leading to brain damage and impairment of internal organs. Hyperbaric therapy removes carbon monoxide and other toxins from the blood much faster than normal breathing, preventing permanent neurological damage and saving lives.
The combination of hyperbaric therapy and skin grafts
If the burn has destroyed the deep layers of the skin and it cannot regenerate on its own, the doctor may recommend a skin graft, in which a portion of healthy skin is taken from another part of the body and transplanted onto the burned area. Hyperbaric therapy also plays an essential role in this process, because:
- It improves vascularization in the graft area, which increases the chances of the transplanted skin taking hold.
- It reduces postoperative inflammation, shortening recovery time.
- It decreases the risk of graft rejection, ensuring faster integration of the transplanted skin.
Hyperbaric therapy has become one of the most valuable complementary methods in treating severe burns, offering patients a faster recovery and significantly reducing the risk of complications. As research continues to demonstrate its benefits, this therapy is increasingly integrated into major burn centers and used to save as much viable tissue as possible, preventing infections and improving the chances of complete recovery.
Treatments for infected burns
If the burn becomes redder, swollen, releases pus, has an unpleasant odor, or is accompanied by fever and chills, a doctor should be consulted as soon as possible. An untreated infection can lead to serious complications and may require intensive treatment. Treatment varies depending on the severity of the infection and the degree of the burn, but generally includes the following measures:
-
Cleaning and wound care
The first step in treating an infected burn is careful cleaning of the affected area. The doctor will remove dead or necrotic tissues through a process called debridement, which helps prevent the spread of bacteria. Regular cleaning with antiseptic solutions, such as chlorhexidine or saline solution, is essential to keep the area as sterile as possible. -
Application of antimicrobial ointments
To combat the infection, antibiotic creams and ointments are used, such as Silver Sulfadiazine or Mupirocin. These help destroy bacteria and protect the skin against additional infection. -
Administration of oral or intravenous antibiotics
If the infection has spread beyond the burn area or there are signs of systemic infection (fever, chills, extensive redness, pus), the doctor will prescribe oral or intravenous antibiotics, depending on severity. The type of antibiotic is chosen based on the bacteria identified through wound cultures. -
Hyperbaric therapy
For infected burns that are healing slowly or show necrosis, hyperbaric therapy can be used to improve tissue oxygenation and combat severe infections, especially those caused by anaerobic bacteria, which develop in oxygen-poor environments. This method helps reduce inflammation, stimulates tissue repair, and accelerates healing. -
Skin grafts for severe burns
If the infected burn has destroyed a large part of the skin and cannot regenerate, the doctor may recommend a skin graft. This involves transplanting healthy skin from another part of the body to cover the affected area and prevent the spread of infection.
Complications of burns

Complications of burns can range from minor problems, such as scarring, to serious life-threatening situations. One of the most common complications is infection, as burned skin loses its role as a protective barrier against bacteria. If the infection spreads, it can lead to septicemia, a serious condition in which bacteria enter the bloodstream and can affect internal organs.
Another major problem is fluid loss and electrolyte imbalance, especially in the case of extensive burns. When a large surface of the skin is damaged, the body rapidly loses water and essential salts, which can lead to dehydration, low blood pressure, and even shock. In such cases, patients must receive intravenous fluids to prevent organ failure.
Over time, severe burns can cause permanent scarring and loss of mobility, especially if they affect areas near joints. Rigid scar tissue can limit movements, and in some cases, medical recovery or surgical interventions are necessary to improve skin flexibility. In addition to physical effects, many people who suffer severe burns also face emotional problems, such as anxiety, depression, or loss of self-confidence, especially if burns affect the face or other visible areas of the body.
The most serious complications of burns are those that affect the entire body and endanger life. Hypovolemic shock is a critical complication, caused by massive fluid loss through burned skin. This leads to a sudden drop in blood pressure, affecting blood circulation and organ oxygenation. If not rapidly intervened with intravenous fluids and specialized treatment, the patient may suffer irreversible damage to vital organs.
In the case of severe burns, compartment syndrome can also occur, a serious condition in which the swelling of tissues in a burned area puts pressure on blood vessels and nerves, blocking circulation. This can lead to tissue death and may require amputation of the affected limb. Also, patients who have inhaled smoke or toxic gases during a fire may suffer respiratory failure, as the lungs are affected by internal burns, which may require mechanical ventilation to maintain vital functions.
Methods for preventing burns
Burns can be prevented through simple safety measures, adapted depending on the type of exposure. Whether it's contact with hot objects, chemicals, electric current, or solar radiation, following basic rules can significantly reduce the risk of injury. Here are the most effective prevention methods for each category of burns:
Prevention of thermal burns
To avoid burns caused by fire, hot liquids, or sharp objects, it's important to be careful in the kitchen, not to leave hot liquids unattended, and to use protective gloves when handling hot objects. At home, it is recommended to set the maximum water temperature at the boiler below 50°C, to prevent scalding. If you use fireplaces, stoves, or other heat sources, make sure they are well protected and that there are no flammable materials nearby.
Prevention of chemical burns
To reduce the risk of chemical burns, it is essential to carefully handle dangerous substances, wearing gloves, protective glasses, and appropriate clothing. Aggressive cleaning products, solvents, and acids should be stored in safe places, out of children's reach. Before use, always read product labels and avoid mixing chemicals, as some combinations can produce dangerous reactions.
Prevention of electrical burns
To avoid electrocutions and electrical burns, it is important to not touch damaged cables or outlets and not to use electrical appliances with wet hands. Electrical installations should be checked periodically to prevent short circuits, and children should be kept away from exposed outlets. Outdoors, contact with high-voltage wires should be avoided, and protective equipment should be used when working near them.
Prevention of sunburns
To avoid sunburns, it is essential to use sunscreen with a minimum SPF 30 factor, especially between 10:00 and 16:00, when UV rays are strongest. Wearing long-sleeved clothing, hats, and sunglasses helps reduce exposure. It is recommended to avoid prolonged sun exposure and to stay constantly hydrated, as dehydration can increase skin sensitivity to burns.
Frequently asked questions and myths about burns
Burns are among the most common domestic accidents, and there are numerous questions and myths circulating around them. Some traditional advice can be useful, but others are completely wrong and can worsen injuries. Here are some of the most common questions and myths about burns:
-
Should I apply butter, oil, or toothpaste to a burn?
❌ Myth: Applying butter, oil, or toothpaste helps heal the burn.
✅ Truth: These substances can trap heat in the skin and worsen the burn. The best immediate treatment is holding the affected area under cold water for 10-15 minutes -
Is ice the best solution to soothe a burn?
❌ Myth: Applying ice to a burn helps cool the skin quickly and relieve pain.
✅ Truth: Ice can cause frostbite and can worsen tissue damage. It's best to use cold water, not ice -
If the burn doesn't hurt, does it mean it's not serious?
❌ Myth: Lack of pain means the burn is not serious.
✅ Truth: A very serious burn can destroy nerve endings, which means the affected area no longer feels pain. If the skin is whitish, brown, or charred and the person feels nothing, it's a sign that the burn is severe and requires urgent medical assistance. -
Should blisters be popped to speed healing?
❌ Myth: Breaking blisters helps the skin heal faster.
✅ Truth: Blisters act as a natural barrier against infections. If they are broken, the exposed area becomes vulnerable to bacteria. It's better to let them heal on their own or, if they break accidentally, to clean the area well and cover it with a sterile dressing. -
Are all sunburns harmless and go away on their own?
❌ Myth: A sunburn is just a cosmetic problem and has no long-term effects.
✅ Truth: Repeated exposure to sunburns can increase the risk of skin cancer and can cause premature skin aging. Even if a sunburn heals, the effects of UV radiation on skin DNA are cumulative. -
If you get burned by an electrical wire and have no visible signs on your skin, do you have no problem?
❌ Myth: If the skin doesn't show visible wounds, the electrical burn is not serious.
✅ Truth: Electrical burns can cause internal injuries, affecting muscles, nerves, and even the heart. Even if you don't see anything on the surface, it's important to see a doctor for an evaluation. -
If you get burned with a chemical substance, should you apply a neutralizing solution?
❌ Myth: If you get burned with an acid, you should apply a base (e.g., baking soda), and if you get burned with a base, you should apply an acid (e.g., vinegar) to neutralize the substance.
✅ Truth: Applying another chemical substance can worsen the burn and can cause an unpredictable chemical reaction. The best treatment is to rinse the affected area with plenty of water for at least 20 minutes and to see a doctor if the burn is serious. -
If you have a severe burn, should you remove clothes stuck to the skin?
❌ Myth: Burned or skin-stuck clothes should be removed immediately.
✅ Truth: Forcibly removing clothes can tear burnt skin and worsen the wound. If clothes are not stuck, you can remove them, but if they are attached to the skin, it's better to wait for medical help. -
Can severe burns heal completely without scars?
❌ Myth: With good treatment, any burn heals without scars.
✅ Truth: Deep burns leave permanent scars, and sometimes skin grafts or special treatments are needed to improve the skin's appearance. Hyperbaric therapy, laser treatments, and special creams can help reduce scarring, but the skin does not completely return to its initial state. -
If you put egg white on a burn, does it help heal?
❌ Myth: Egg white has soothing properties and helps regenerate burned skin.
✅ Truth: Applying egg white to a burn can introduce bacteria into the wound and increase the risk of infection, especially if the egg is raw and contaminated with Salmonella. The safest treatment is cooling the burn with cold water and applying a sterilized ointment. -
If you apply alcohol or rubbing alcohol to a burn, do you disinfect it faster?
❌ Myth: Rubbing alcohol or alcohol helps prevent infections and accelerates healing.
✅ Truth: Alcohol can irritate burned skin even more, causing pain and delaying the healing process. Disinfecting a burn should be done with saline solution or a mild antiseptic, not with alcohol. -
If you burn your tongue, should you suck on ice to calm the pain?
❌ Myth: Ice immediately reduces inflammation and helps healing.
✅ Truth: Ice applied directly to a burn can cause frostbite and can worsen the injury. Instead, it's better to drink small sips of cool water or consume soft and cold foods, such as yogurt or milk, to soothe the pain. -
If you have severe sunburns, should you take a hot shower to "open the pores"?
❌ Myth: Hot water helps the skin eliminate toxins and recover faster.
✅ Truth: A hot shower worsens inflammation and increases discomfort. It's best to take a shower with lukewarm or cool water, to soothe the skin and reduce redness. -
If you get burned, should the wound be exposed to air to heal faster
❌ Myth: Burns heal faster if left uncovered.
✅ Truth: Leaving a burn exposed increases the risk of infection and can lead to excessive drying of the skin, delaying healing. It is recommended to apply a sterile dressing and keep the skin hydrated for faster recovery.
Myths about burns have been passed down from generation to generation, but many of them can do more harm than good. Using wrong home remedies, such as applying butter, flour, or ice, not only doesn't help but can worsen the burn or slow healing. Also, concepts such as "if it doesn't hurt, it's not serious" or "breaking blisters helps" are dangerous ideas that can lead to infections and serious complications.
For proper care, it's important to rely on proven medical advice and apply safe methods, such as cooling the burn with cold water, protecting the area with sterile dressings, and seeking medical help for severe burns. Avoiding myths and applying correct treatment can make the difference between rapid healing and complications that could be prevented.




